Group Health Insurance
Health Insurance plans come in various classifications for every single organisation and group health
insurances. The main intent of a Group Health Insurance plan is to provide risk coverage
to people belonging to a same group.Companies often use the group health insurance plan
as a tool to improve retention ratio in their organisations. This helps the company to
instill confidence amongst their employees which in return helps the company to extract
more out of their employees. Usually, majority of the companies offer group health
insurance plan to establish and offer protection to the employees and their family
members, suffered in the business organisation. For employees, it is regarded as an
essential requirement which is also offered with more benefit to the
employee.
This kind of policy is generally provided by:
1. An employer to the employee
2. Banks to their Credit Card Holders or Account Holders
3. Clubs or Gyms
4. Any Corporate or Organisations
The size of the group and premium payable may vary from organisation to organi-sation,
as it depends on the nature of cover and the demographic composition of the group size.
However, the pricing of such group health insurance plans are discounted in comparison
with retail health insurances.
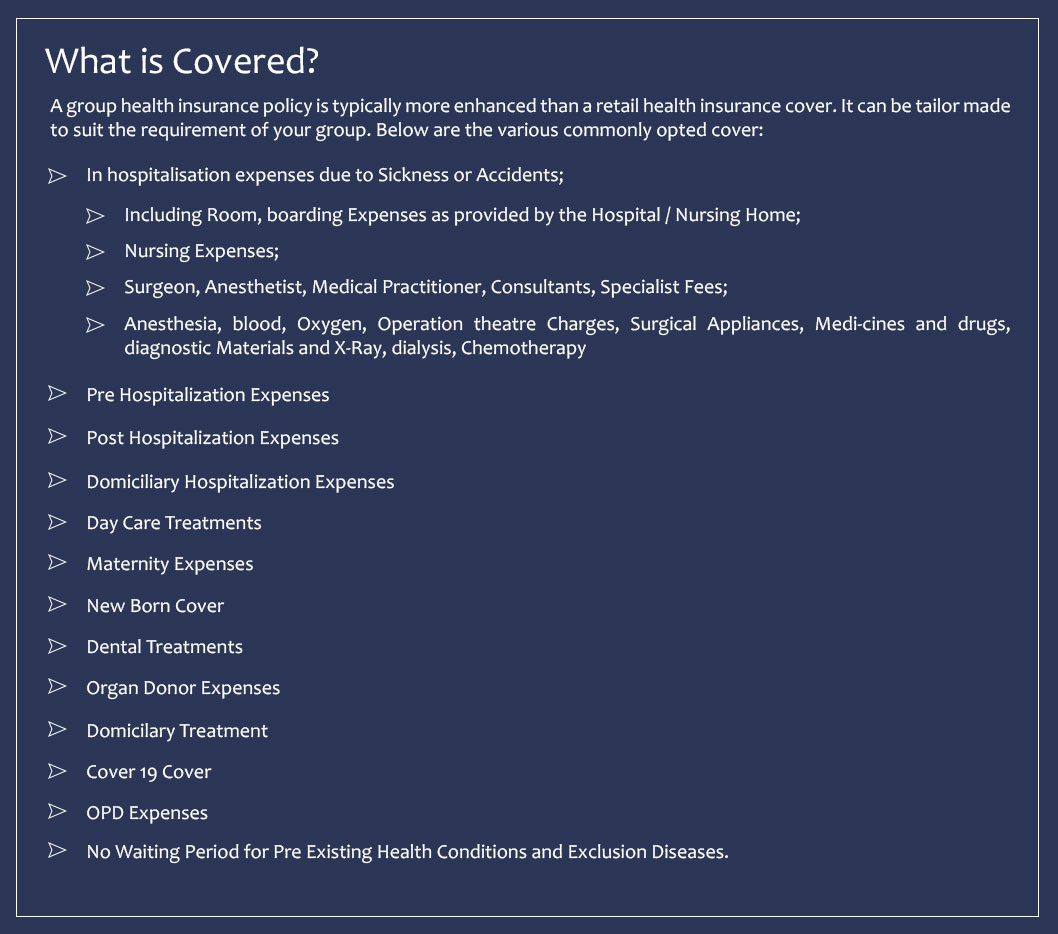
What is Covered?
A group health insurance policy is typically more enhanced than a retail
health insurance cover. It can be tailor made to suit the requirement of
your group. Below are the various commonly opted cover:
- In hospitalisation expenses due to Sickness or
Accidents
- Including Room, boarding Expenses as provided by the Hospital / Nursing Home;
- Nursing Expenses;
- Surgeon, Anesthetist, Medical Practitioner, Consultants, Specialist Fees;
- Anesthesia, blood, Oxygen, Operation theatre Charges, Surgical Appliances, Medi-cines and drugs, diagnostic Materials and X-Ray, dialysis, Chemotherapy
- Pre Hospitalization Expenses
- Post Hospitalization Expenses
- Domiciliary Hospitalization Expenses
- Day Care Treatments
- Maternity Expenses
- New Born Cover
- Dental Treatments
- Organ Donor Expenses
- Domicilary Treatment
- Cover 19 Cover
- OPD Expenses
- No Waiting Period for Pre Existing Health Conditions and Exclusion Diseases.


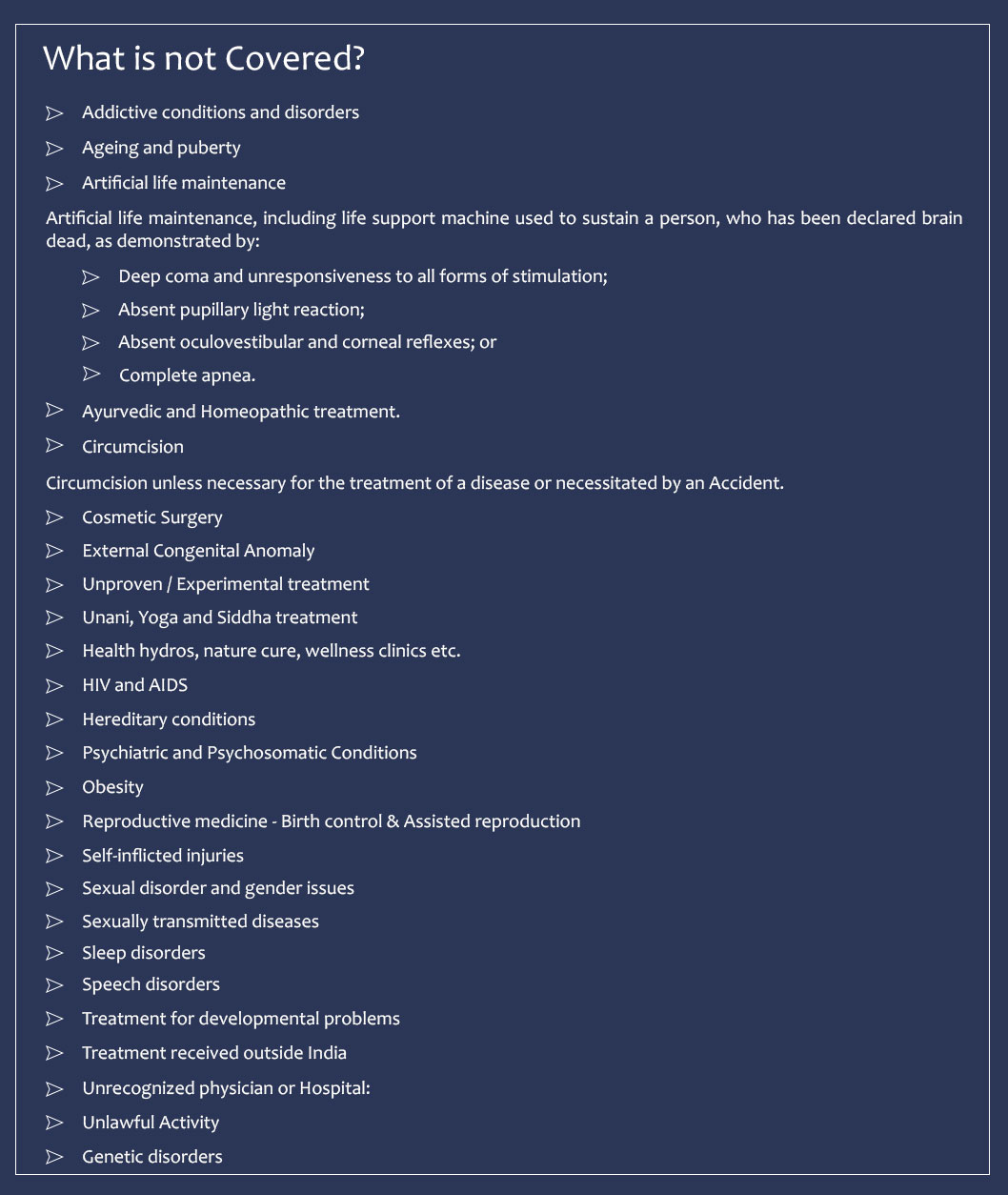
What is not covered?
- Addictive conditions and disorders
- Ageing and puberty
- Artificial life maintenance
- Deep coma and unresponsiveness to all forms of stimulation;
- Absent pupillary light reaction;
- Absent oculovestibular and corneal reflexes; or
- Complete apnea.
- Ayurvedic and Homeopathic treatment.
- Circumcision
- Cosmetic Surgery
- External Congenital Anomaly
- Unproven / Experimental treatment
- Unani, Yoga and Siddha treatment
- Health hydros, nature cure, wellness clinics etc.
- HIV and AIDS
- Hereditary conditions
- Psychiatric and Psychosomatic Conditions
- Obesity
- Reproductive medicine - Birth control & Assisted reproduction
- Self-inflicted injuries
- Sexual disorder and gender issues
- Sexually transmitted diseases
- Sleep disorders
- Speech disorders
- Treatment for developmental problems
- Treatment received outside India
- Unrecognized physician or Hospital:
- Unlawful Activity
- Genetic disorders
Artificial life maintenance, including life support machine used to sustain a person, who has been declared brain dead, as demonstrated by:
Circumcision unless necessary for the treatment of a disease or necessitated by an Accident.
How To Get Claims?
- Duly filled claim form
- Original bills, receipts and discharge certificate/card from the Hospital/ Medical Practitioner. (Self attested copies of bills, receipts and Hospital discharge summary can be provided for Critical Illness or Hospital Cash claim)
- Original bills from chemists supported by proper prescription
- Original consultation notes and/or investigation test reports and payment receipts supported by prescription. (Self attested copies of bills, receipts and Hospital discharge summary can be provided for Critical Illness or Hospital Cash claim)
- Medical Practitioner's referral letter advising Hospitalisation in non-accident cases.
- Details of any other insurance policy that may respond to the claim
- First Information Report (FIR) & Panchnama/Medico Legal Certificate for medico-legal cases. (If Applicable)
